The quest for reliable prediction of chemotherapy-induced delayed nausea among breast cancer patients
Abstract
Aim: Though female sex is considered a risk factor when predicting chemotherapy-induced nausea, not all women will experience nausea. Therefore, the aim of this pilot study was to evaluate the accuracy, and usefulness, of a blood-based assay for predicting chemotherapy-induced delayed nausea among breast cancer patients.
Methods: Whole blood from consented breast cancer patients, determined to benefit from chemotherapy, were used to test each individual for their intrinsic glutathione recycling capacity. Both highly-emetogenic and moderately-emetogenic chemotherapies were included in the study. Test results obtained from chemotherapy naïve patients were used to predict delayed nausea. Predicted outcomes were later compared to reported outcomes documented in medical records. Statistical analyses were used to test the accuracy and efficacy of our blood-based test.
Results: Even with current and effective anti-emetics, we report that ~31% of breast cancer patients reported delayed nausea. Using the SAS/STAT classification and regression tree method we were able to show that this assay can be used as a predictive tool with an AUC of 0.71-0.74 depending on treatment regimen.
Conclusion: The new predictive assay provides an added value in identifying individual breast cancer patients at high risk of developing moderate or severe delayed nausea after treatment with taxane- based therapies such as docetaxel/cyclophosphamide and docetaxel/carboplatin/trastuzumab/pertuzumab. We believe that this assay could help guide the use of anti-emetics for improved patient-oriented care.
Keywords
Introduction
Nausea and vomiting are some of the most common and feared side effects by cancer patients receiving chemotherapy treatments[1]. Chemotherapy-induced nausea and vomiting (CINV) places a substantial burden on patients and their loved ones, which greatly reduces the quality of life, nutritional habits, ability to work and care for their families, and adherence to treatment regimens[2,3].
Each year approximately 250,000 new cases of breast cancer are diagnosed in the United States of America[4]. Based on stage at time of diagnosis, 38% with stage I/II and 82% of stage III disease will commence chemotherapy treatments to improve their chance of long-term disease-free survival[5]. As a result, assessment of CINV risk represents a major focal point when trying to reduce healthcare costs and societal burdens associated with chemotherapy.
Though CINV in the acute phase (within 24 h of therapy) is mostly controlled with current anti-emetics, the delayed form (occurring 24-72 h post therapy) is still difficult to predict by medical staff and therefore also difficult to prevent[6-8]. Currently, risk assessment of nausea is based primarily on assumptions from known risk factors such as type of chemotherapeutic agent administered, age, and sex, while history of alcohol consumption, motion sickness, or previous complications with general anesthesia or chemotherapy are also considered[7,9-11].
The combination of modern antiemetic drugs and predictive risk factors, particularly female sex and age[11,12], has contributed to a reduction of the incidence of CINV. However, the actual incidence of CINV is still largely underestimated by both clinicians and nurses[7,9]. In a single-institution qualitative study with equal gender distribution, the incidence of CINV was estimated to be nearly 20%[9]. However, the true incidence of CINV among breast cancer patients is likely higher due to a larger proportion being female and possibly of younger age compared to other solid tumors, resulting in a greater predisposition for CINV[7,13]. The duration and severity of delayed nausea has been shown to have the greatest negative impact on quality of life and healthcare costs and warrants urgent attention to prevent the conditioned anticipatory nausea reaction at future treatment visits[13,14] and provide a satisfactory therapeutic outcome for patients[15].
Predicting the incidence and severity of delayed nausea, a subjective sensation, is difficult to assess and quantify as compared to vomiting[16]. Though the pathophysiology of emesis is poorly understood, the emetic response is an evolutionary, protective mechanism in which the body aims to expel toxins, such as chemotherapeutic agents[17]. While the emetogenic pathway appears to be responsible for both vomiting and nausea, some patients will experience nausea without emesis which suggests that nausea may be a low level activation of the pathway whereas vomiting represents a motor response with increased stimulation of the pathway[1]. Alternatively, since CINV is triggered by a complex signaling network, differences in severity of CINV could be affected by the balance between signaling pathways and/or due to personal variation in sensitivity to the triggers of CINV[18]. The underlying mechanism for the therapeutic action of chemotherapies is the induction of cell death, resulting in release of reactive oxygen species (ROS)[19,20]. This burst of ROS triggers the release of neurotransmitters, such as serotonin and substance P, from the enterochromaffin cells found in the upper small intestine[17]. The emetic reflex is then activated when these neurotransmitters bind to the 5-hydroxytryptamine3 (5-HT3) and neurokinin-1 (NK1) receptors, respectively, in the chemoreceptor trigger zone of the central nervous system[16,17,21-24].
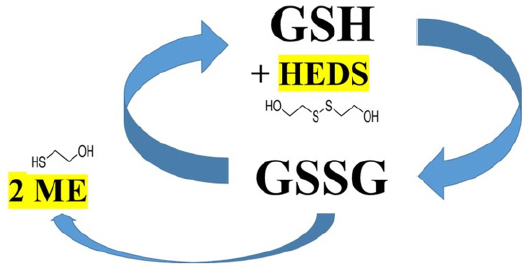
Therefore, we hypothesized that glutathione (GSH), an endogenous antioxidant directly responsible for scavenging and neutralizing ROS, could alleviate the emetic response if it is recycled efficiently[25]. Several enzymatic pathways contribute to the recycling of GSH from its reduced state (GSH) to its oxidized state, glutathione disulfide (GSSG) and then back to GSH[16][Figure 1]. A personal variability could, at least in part, be due to genetic variations such as single nucleotide polymorphisms (SNPs) that have been reported to reduce the enzymatic activity required for glutathione recycling[26,27]. To determine an individual’s recycling capacity, we are using the bioactive probe hydroxyethyl disulfide (HEDS)[28] that is converted to mercaptoethanol by the glutathione recycling pathway [Figure 1]. Measuring the amount of mercaptoethanol produced per time unite will provide an indirect assessment of an individual’s glutathione recycling capacity. Patients with a high glutathione recycling capacity will be predicted to efficiently neutralize ROS, resulting in reduced levels of neurotransmitters and a lessened activation of the emetic pathway. Identifying personalized risk of CINV can aid in the determination of appropriate use of antiemetics, which is critical to high quality cancer care.
Figure 1. Simplified schematic presentation of the glutathione recycling and conversion of hydroxyethyl disulfide (HEDS) to mercaptoethanol (ME). HEDS reacts with glutathione (GSH) and the disulfide bonds are cleaved by the enzymes in the glutathione recycling pathway. The resulting mercaptoethanol can be measured using spectrophotometry and provide an indirect determination of a patient’s ability to recycle glutathione and neutralize reactive oxygen species
The development of receptor antagonists, targeting known emetic receptors, such as 5-HT3 and NK1, has produced good responses in clinical practice. However, these agents also trigger adverse effects that range from constipation and headaches to heart arrhythmias such as prolonged QT[29]. Also, the costs associated with some of these antiemetic drugs might place a financial burden on patients as some may struggle to manage co-payments and deductibles for their chemotherapy[6,30]. Thus, there is a medical and financial need to stratify patients who are at high or low risk of developing delayed nausea so that appropriate antiemetics can be prescribed to those who need it the most[31].
Here, we report on the preliminary evaluation of the glutathione recycling capacity (GRC) assay as a predictive tool for delayed chemotherapy-induced nausea among breast cancer patients treated with any of the four most common therapeutic regimens. We have previously shown that this assay can stratify patients treated with platinum-based therapies who are at high vs. low risk of developing delayed nausea[16]. Though the cohort of breast cancer patients is still rather small, the results obtained from the statistical analyses are encouraging and match the results from the platinum-treated cohort. Taken together, we believe that this assay might be used as a tool to help clinicians personalize treatment plans to better care for patients at risk of developing delayed nausea.
Methods
Patient cohort
Chemotherapy naïve patients seeking medical care at Lankenau Medical Center Cancer Center for a diagnosis of breast cancer were asked to participate in this on-going prospective study approved by our local Institutional Review Board. Written and signed informed consent was obtained from all patients prior to obtaining blood specimens. The approved protocol allows all adults (at least 18 years of age) of both sexes to participate in the study. All patients were treated according to current medical standards; where choices were available, the medical staff had exclusive authority in recommending therapy based on patient-related matters, such as stage of disease and/or possible co-morbidities. Exclusion criteria included any prior chemotherapy, radiation therapy given within three months, current use of glutathione-containing supplements, and inability to provide written consent.
Patients diagnosed with hormone receptor (HR) positive disease were mainly treated with a moderately emetogenic chemotherapy (MEC) containing a taxane (docetaxel) while those with HR-negative and HER2-negative disease predominantly received a highly emetogenic chemotherapy (HEC) including an anthracycline agent therapy. HER2-positve patients were typically treated with docetaxel and carboplatin combined with trastuzumab (TCH) as adjuvant therapy while in the neoadjuvant setting HER2-positive patients received docetaxel and carboplatin with concurrent trastuzumab and pertuzumab (TCHP). In combination therapies, the agent with the highest emetogenic potential will guide the designation of the regimen. The TCH and TCHP are therefore usually considered MECs.
Glutathione recycling capacity
Each patient donated a tube of blood [12 mg K2EDTA (“purple top”)] prior to each treatment cycle. All samples were kept at +4 °C and assayed within 24 h. The GSH recycling capacity in red blood cells was measured using whole blood and reagents from a commercially available kit (OxPhosTM Cell Survival Kit, cat. no. KLD-02, Rockland Inc.). In brief, this assay uses hydroxyethyl disulfide (HEDS) as an indirect indictor of glutathione-dependent detoxification involving conversion of GSH→GSSG→GSH, which converts HEDS into mercaptoethanol (ME) [Figure 1] that can be quantified with dithiobisnitrobenzoic acid (DNTB)[28]. As previously described[16], aliquots of whole blood from patients were incubated with the HEDS reagent and final supernatants were mixed with DNTB reagents allowing levels of produced ME to be determined in a spectrophotometer at 412 nm (Beckman Coulter DU® 730). Following the vendor instructions, absorbance readings were converted into ME concentrations and then normalized to total red blood cell count (RBC × 106), as determined at the time of blood draw using a Sysmex XN-1000 in the clinical lab.
Glutathione recycling capacity as predictive marker
Samples collected from chemotherapy naïve patients were used to predict nausea risk. Additional samples collected during therapy served to assess possible effect of chemotherapy on the recycling capacity. As part of standard of care, adverse symptoms such as nausea and vomiting are monitored and recorded in medical records by each medical oncologist. In accordance with the CTCAE Adverse Events Guide of 2017[32] “no nausea” was given a score of 0 while mild symptoms that required no intervention were given a score of 1. Moderate symptoms that mandated additional interventions were given a score of 2 while severe, but not life-threatening symptoms, were scored as 3.
Statistical methods
Reported levels of nausea were analyzed against chemotherapeutic agent, recycling capacity, and age. Two of the patient characteristics frequently used to predict nausea are age and sex. Currently, this study consists of 99.25% female patients and therefore does not permit a stratification based on sex. All analyses were made using the SAS/STAT v 14.1 classification and regression trees (CART) method[33]. Using this method, we obtained values for sensitivity, specificity, and misclassification rate. The area-under-curve (AUC) was used as a measurement of the accuracy of the test.
Results
Subject accrual
This study was conducted at the Lankenau Institute for Medical Research, located on campus of the Lankenau Medical Center (LMC) in Wynnewood, a suburb of Philadelphia, PA. In total, 205 patients being treated with any of the common chemotherapies for breast cancer at the LMC Cancer Center have provided written consent to participate in the study. The treatments given were based on tumor characteristics and possible comorbidities.
Patient demographics
For this study, all patients treated with anthracycline, taxane, TCH and TCHP were included in this preliminary assessment of the GRC assay. Anthracyclines are reported to induce cardiotoxicities, which is why clinicians tend to avoid treating older patients with this agent. Therefore, to prevent age, a commonly used predictive risk factor of nausea, to impact the evaluation of the GRC assay we selected age-matched patients among those treated with taxane-based therapy to create a cohort of similar size. Thus, this report is based on 133 patients from the complete cohort of enrolled patients. With the focus on breast cancer patients, the sex distribution in the study was predominantly female [n = 132 (99.25%)]; however, there was one male patient included [n = 1 (0.75%)]. Mean age was 54.49 years old (range 23 to 85 years old) while the median age was 55 years old. In total, 97 patients (72.93% of the total cohort) identified as Caucasian, whereas 31 (23.31%) identified as African-American. Due to the geographical proximity of LMC to West Philadelphia, with a predominantly African-America population (72%)[34], the study cohort has a higher than national average (13.4%) number of participating patients of African-American descent[35]. Other races and ethnicities contributed < 1% each to the overall cohort.
Median age of the 42 patients treated with an anthracycline-based therapy [Table 1] was 55.5 years with an age range of 25 to 69 year of age. Anthracyclines are considered HEC agents and thus all patients received a three-agent prophylactic antiemetic treatment prior to infusion. The race distribution within this sub-group is near identical to that of the entire cohort.
Cohort characteristics for patients treated with anthracycline-based therapy
| Anthracycline-based | Patients (%) | Number of patients | |
|---|---|---|---|
| Characteristics | |||
| Anthracycline-treated number of patients (Total)* | 42(133) | ||
| Age (M ± SD) | 52.10 ± 11.5 | ||
| Median age (Range) | 55.5 (25-69) | ||
| Sex | |||
| Female | 100.00% (99.25%) | 42(132) | |
| Male | 0.00% (0.75%) | 0(1) | |
| Race | |||
| Caucasian | 76.19% (72.93%) | 32(97) | |
| African American | 19.05% (23.31%) | 8(31) | |
| Other | 4.76% (3.76%) | 2(5) | |
| Antiemetic medications (n = 42) | |||
| Prior to chemotherapy | |||
| Palonosetron (Aloxi) 0.25 mg | 100.00% | 42 | |
| Dexamethasone | 100.00% | 42 | |
| Aprepitant (Emend) | 100.00% | 42 | |
| Home antiemetics prior to treatment | |||
| Ondansetron (Zofran) 8 mg | 85.71% | 36 | |
| Prochlorperazine (Compazine) | 78.57% | 33 | |
| Dexamethasone | 76.19% | 32 | |
| Home antiemetics added later | |||
| Ondansetron (Zofran) 8 mg | 14.29% | 6 | |
| Prochlorperazine (Compazine) | 11.90% | 5 | |
| Aprepitant (Emend) | 0.00% | 0 | |
| Dexamethasone | 7.14% | 3 | |
The median age among the 39 patients treated with a taxane-based regimen, age-matched to the anthracycline-based therapy group, was 56 as compared to 55.5 for the previous group. Though the median age is similar for these two groups, the age range demonstrates how clinicians favor taxane-based therapy for older patients, 36-85 for taxane-based vs. 25-69 for anthracycline-based [Tables 1 and 2]. Again, there is no significant difference in race distribution in this sub-group compared to the whole cohort. This sub-group was predominantly given a two-agent combination consisting of 5-HT3 antagonist and steroids as antiemetic prophylaxis and had less need for rescue antiemetics post-therapy compared to the anthracycline-based treated group.
Cohort characteristics for patients treated with taxane-based therapy
| Taxane-based | Patients (%) (% of non-taxane treated patients) | Number of patients | |
|---|---|---|---|
| Characteristics | |||
| Number of patients | 39 | ||
| Age (M ± SD) | 56.69 ± 13.9 | ||
| Median age (Range) | 56 (36-85) | ||
| Sex | |||
| Female | 100.00% | 39 | |
| Male | 0.00% | 0 | |
| Race | |||
| Caucasian | 71.79% | 28 | |
| African American | 28.21% | 11 | |
| Other | 0.00% | 0 | |
| Antiemetic medications (n = 38) | |||
| Prior to chemotherapy | |||
| Palonosetron (Aloxi) 0.25 mg | 94.74% (95.8%)* | 36 | |
| Dexamethasone | 97.37% (95.8%) | 37 | |
| Aprepitant (Emend) | 7.89% (48.9%) | 3 | |
| Home antiemetics prior to treatment | |||
| Ondansetron (Zofran) 8 mg | 89.47% (88.5%) | 34 | |
| Prochlorperazine (Compazine) | 78.95% (83.3%) | 30 | |
| Dexamethasone | 92.11% (75%) | 35 | |
| Home antiemetics added later | |||
| Ondansetron (Zofran) 8 mg | 2.63% (7.3%) | 1 | |
| Prochlorperazine (Compazine) | 0.00% (8.3%) | 0 | |
| Aprepitant (Emend) | 0.00% (1.0%) | 0 | |
| Dexamethasone | 0.00% (5.2%) | 0 | |
The cohort treated with TCH consisted of 27 patients with a median age 62 years old (range 34-72)
Again, there was no difference in race distribution between the subgroup and the full cohort [Table 3]. Though, the TCH therapy includes an anti-HER2 targeted agent that reportedly can induce the development of cardiotoxicities, this group had a higher median age compared to the anthracycline-based therapy group. Similar to the taxane-based treated group, the majority of patients received a two-agent combination antiemetic preventive treatment.
Cohort characteristics for patients treated with taxane/carboplatin/trastuzumab-based therapy
| TCH-based | Patients (%) | Number of patients | |
|---|---|---|---|
| Characteristics | |||
| Number of patients | 27 | ||
| Age (M ± SD) | 58.11 ± 10.91 | ||
| Median age (Range) | 62 (34-72) | ||
| Sex | |||
| Female | 100.00% | 27 | |
| Male | 0.00% | 0 | |
| Race | |||
| Caucasian | 74.07% | 20 | |
| African American | 22.22% | 6 | |
| Other | 3.70% | 1 | |
| Antiemetic medications (n = 27) | |||
| Prior to chemotherapy | |||
| Palonosetron (Aloxi) 0.25 mg | 92.59% | 25 | |
| Dexamethasone | 92.59% | 25 | |
| Aprepitant (Emend) | 7.41% | 2 | |
| Home antiemetics prior to treatment | |||
| Ondansetron (Zofran) 8 mg | 92.59% | 25 | |
| Prochlorperazine (Compazine) | 85.19% | 23 | |
| Dexamethasone | 85.19% | 23 | |
| Home antiemetics added later | |||
| Ondansetron (Zofran) 8 mg | 3.70% | 1 | |
| Prochlorperazine (Compazine) | 7.41% | 2 | |
| Aprepitant (Emend) | 3.70% | 1 | |
| Dexamethasone | 0.00% | 0 | |
The last sub-group was treated with neoadjuvant TCHP for HER2-postive disease and consisted of 25 patients with a median age of 52 years. All patients in this group received at least two antiemetic agents prior to infusion but a three-agent combination at home the days before treatment. Though this combination does not include a HEC agent, reports from the CLEOPATRA trial[36] reported an increased risk of nausea that might persuade the additional antiemetics used in this group. The minor shift in the race distribution seen in Table 4, it is not statistically significant.
Cohort characteristics for patients treated with taxane/carboplatin/trastuzumaband pertuzumab-based therapy
| TCHP-based | Patients (%) | Number of patients | |
|---|---|---|---|
| Characteristics | |||
| Number of patients | 25 | ||
| Age (M ± SD) | 51.16 ± 10.93 | ||
| Median age (Range) | 52 (23-69) | ||
| Sex | |||
| Female | 96.00% | 24 | |
| Male | 4.00% | 1 | |
| Race | |||
| Caucasian | 68.00% | 17 | |
| African American | 24.00% | 6 | |
| Other | 8.00% | 2 | |
| Antiemetic medications (n = 25) | |||
| Prior to chemotherapy | |||
| Palonosetron (Aloxi) 0.25 mg | 100.00% | 25 | |
| Dexamethasone | 100.00% | 25 | |
| Aprepitant (Emend) | 12.00% | 3 | |
| Home antiemetics prior to treatment | |||
| Ondansetron (Zofran) 8 mg | 96.00% | 24 | |
| Prochlorperazine (Compazine) | 96.00% | 24 | |
| Dexamethasone | 88.00% | 22 | |
| Home antiemetics added later | |||
| Ondansetron (Zofran) 8 mg | 4.00% | 1 | |
| Prochlorperazine (Compazine) | 4.00% | 1 | |
| Aprepitant (Emend) | 0.00% | 0 | |
| Dexamethasone | 8.00% | 2 | |
Incidence of nausea
The overall incidence of moderate-to-severe delayed nausea was determined by the number of patients who reported nausea during office visits and was classified by medical oncologist as severity score 2 or 3 according to CTCAE Adverse Events Guide of 2017[32]. Across all treatment groups, 42 of 133 patients reported moderate-to-severe delayed nausea resulting in an overall incidence of 31.58%. The highest incidence of nausea was reported by patients given the HEC designated anthracycline-based therapy followed by the TCHP regimen. The lowest incidence of nausea was reported by patients in the TCH-based therapy group.
Evaluation of GRC as predictive tool for delayed nausea
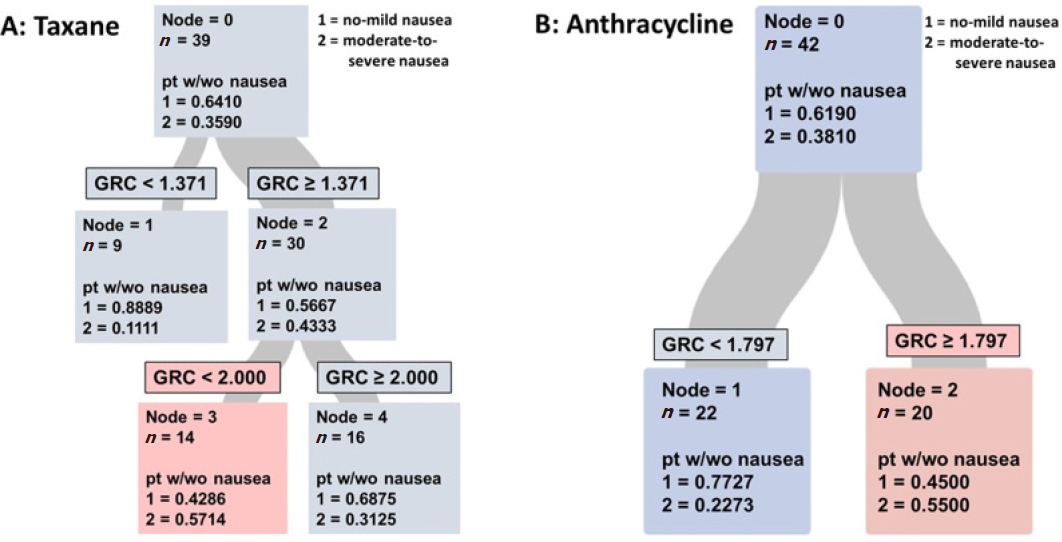
To evaluate the GRC assay as a predictive tool for breast cancer patients, we used the CART algorithm in the SAS/STAT statistical program. The CART algorithm is a regression model that selects a single stratification variable in order to define cutoff values for various datasets[33]. By doing so, the CART algorithm determines which variable is most important to create two, binary children nodes from a parent node with the highest homology with respect to the best predictor variable[33]. The parent node is labeled Node = 0, while each child node is labeled Node = 1 and Node = 2. In this analysis the score 1 represents the proportion of each node that experienced no-to-mild delayed nausea while score 2 represents the proportion who suffered from moderate-to-severe delayed nausea.
Nausea prediction for patients treated with taxane-based therapy
The results from the CART analysis of the taxane-based treated cohort is shown in Figure 2A. The parent node in the figure represents all 39 patients treated with a taxane-based therapy. Of these patients, 35.90% reported moderate-to-severe delayed nausea after treatment with this MEC regimen. The algorithm then spilt the cohort into two groups using the best predictor variable, which was found to be GRC, generating two child nodes with increased homology. The first cutoff-point identified by the program was 1.371 mmol/L ME/RBC. As seen in Figure 2A, the majority of the patients with a GRC value of less than 1.371 (~89%) experienced no or mild nausea.
Figure 2. Classification and regression trees evaluation of glutathione recycling capacity (GRC) as predictive factor for patients treated with taxane-based (A) or anthractcline-based (B) chemotherapy. For patients treated with taxane-based therapies, the GRC assay provides a better risk stratification than age while it does not aid in identifying patients at risk among those treated with anthracycline-based therapies
The other node (Node 2), consisted of 30 patients with a GRC values above 1.371 mmol/L ME/RBC and an almost even split between the two nausea levels. For the purpose of this preliminary evaluation, 30 patients were determined to be sufficient for further analysis and the algorithm provided a second cutoff-point to better classify the larger child node. A second cutoff point of 2.0 mmol/L ME/RBC was identified and spilt the cohort into 14 patients with GRC between 1.371-2.000 mmol/L ME/RBC and 16 patients with GRC greater than 2.0 mmol/L ME/RBC. Interestingly, using this second cut-off point correctly predicted the moderate-to-severe nausea for 8 of the 14 (57.14%) patients with intermediate GRC values, and 11 of the 16 (68.75%) patients with no-to-mild nausea with a GRC higher than 2.0 mmol/L ME/RBC. The area-under-curve (AUC) for the GRC assay as predictive marker was 0.7071 (sensitivity 0.5714 and specificity 0.7600) with a misclassification rate of 0.3077.
Anthracycline-based treatment cohort
Using the same approach as for patients treated with taxane-based therapies, the CART method identified the GRC as the best predictor variable for patients treated with anthracycline-based therapies. The overall incidence of moderate-to-severe delayed nausea was 38.10% in this group. Again, the CART method tailored the cut-off point to create child nodes with increasing homology. Of the patients in node 1, with a GRC test result below the cut-off point of 1.797 mmol/L ME/RBC, 77.2% were identified as low risk for moderate-to-severe nausea. Of the patients (n = 20) with a GRC greater than 1.797 mmol/L ME/RBC, 55.00% reported moderate-to-severe delayed nausea. The overall sensitivity was 0.6875 while the specificity was 0.6538. The AUC for the cohort was 0.6707 with a misclassification rate of 0.3333 indicating that the GRC assay is not likely to provide reliable predictions of delayed nausea for patients treated with anthracyclines.
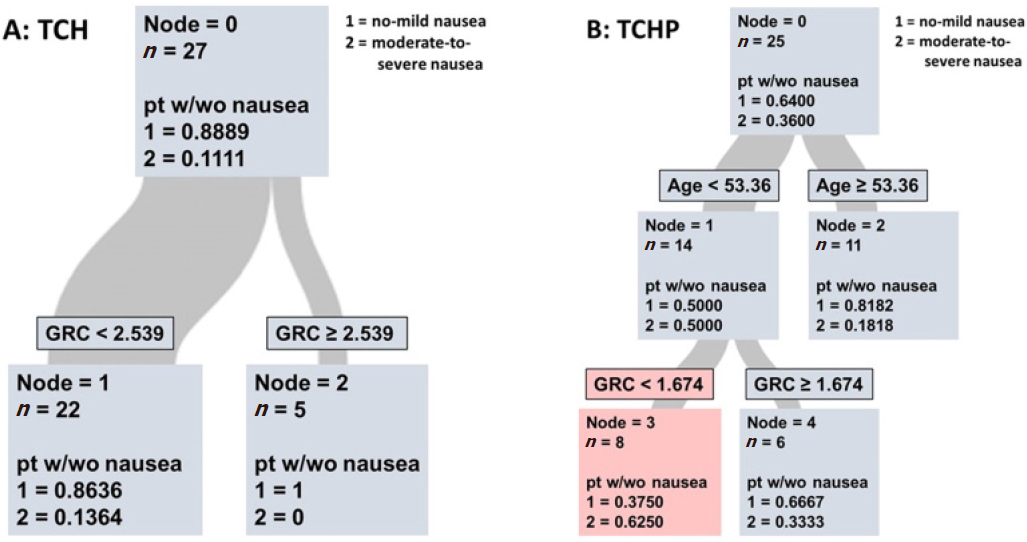
GRC assay as biomarker for nausea in combination regimens
There are two common treatment regimens for HER2-positive breast cancers that both include a taxane and a platinum agent, TCH and TCHP. These two regimens both contain taxane and carboplatin that are classified as MEC agents while the HER2 targeting agents are classified as low emetogenic chemotherapies (LEC)[30]. At first these two groups were pooled but upon realizing the prominent difference in nausea incidence between the two regimens, 11% in TCH vs. 36% in TCHP, we again separated patients based to treatment regimen [Figure 3].
Figure 3. Classification and regression trees evaluation of glutathione recycling capacity (GRC) as predictive tool for patients treated with TCH (A) or TCHP (B) chemotherapy. As seen in A, GRC has no added value for risk stratification. In contrast, when breast cancer patients are first separated into young/older age, the GRC can aid in the identification of individuals at high risk for moderate-to-severe delayed nausea
Using the same algorithm, the cutoff-point for the TCH-based cohort was determined to be 2.539 mmol/L ME/RBC [Figure 3A]. However, only a very low total number of patients experienced nausea (n = 3) induced by TCH and the GRC assay did not identify these patients as seen by the sensitivity of 0.0000 and specificity of 1.00.
TCHP-based treatment cohort
In the TCHP regimen group 36.00% of patients reported moderate-to-severe delayed nausea [Figure 3B]. In this group the GRC assay was not the better predictor variable but rather age was. However, when the statistical program divided patients into “younger” (< 53.36 years old) and older (> 53.36 year old) prior to applying the GRC assay, 62.5 % of patients in the younger set [Figure 3B] and with a GRC score below 1.674 had their risk of moderate-to-severe nausea correctly predicted. In the older cohort, 81.82% reported no-to-mild delayed nausea responses which is consistent with previous research suggesting the incidence of delayed nausea decreases with increasing age[8]. Of the patients in the younger cohort, 66.67% were correctly classified with a GRC score above the cutoff as having no-to-mild delayed nausea. The sensitivity was determined as 0.5560 with a specificity of 0.8125. The AUC was 0.7188 and the misclassification rate was 0.2800.
As seen in the summary table [Table 5], based on the AUC values for the GRC assay, though not perfect, provide a better individual prediction than age for patients treated with a taxane-based or TCHP regimen. At this point, very few patients have reported moderate-to-severe nausea in the TCH cohort and we cannot make any assessment of the assay for this treatment group. The cut-off value for the two groups where the assay shows the greatest promise as predictive marker, taxane-based and TCHP regimen, are in the same range, 1.371-2.00- and ≤ 1.674, respectively. The algorithm tailored cutoff value for the anthracycline-based treated cohort is in a similar range but does not provide as a reliable prediction as seem for the other two regimens.
Summary of statistical evaluation of glutathione recycling capacity assay as predictive marker for delayed nausea induced by the four most common chemotherapies for the treatment of breast cancer
| Treatment | Sensitivity | Specificity | AUC | Misclassification rate |
|---|---|---|---|---|
| Taxane-based | 0.5714 | 0.7600 | 0.7071 | 0.3077 |
| Anthracycline-based | 0.6875 | 0.6538 | 0.6707 | 0.3333 |
| TCH | 0.0000 | 1.0000 | 0.7431 | 0.1111 |
| TCHP | 0.5560 | 0.8125 | 0.7188 | 0.2800 |
Discussion
Breast cancer primarily afflicts women and even though many are spared chemotherapy due to a diagnosis of early-stage and/or hormone receptor positive disease, based on the large number of newly diagnosed cases of breast cancer each year - a significant number of women will nevertheless have to endure chemotherapy and the associated side effects. Among all side effects, nausea is the adverse effect that the majority of patients reportedly fear the most[7]. Nausea is a subjective symptom that can last for days with no objective measurement to predict, gauge, or monitor.
Empirically identified risk factors for nausea include choice of chemotherapeutic agent, female sex, young age, alcohol consumption, previous experience of motion sickness or post-surgery nausea. Of these, the chemotherapeutic agent given is considered to be the strongest predictor followed by sex and age, perhaps due to reliable information regarding these factors. Reports in the literature have demonstrated that 56%-74% of patients can have their risk of delayed nausea correctly classified using these risk factors in algorithms and prediction indexes[37,38]. While this approach provides some general guidance, both clinicians and nurses still frequently underestimate the incidence of nausea[7,8] leaving some patients undertreated while others might be over-treated, subjecting the latter group to agents that are not without side effects.
In order to address this problem, we focused our current study on a quantifiable blood assay, based the glutathione recycling capacity of red blood cells, that our previous study[16] demonstrated can serve as a predictive tool in a mixed gender cohort consisting of lung and colon patients treated with platinum-based chemotherapy.
With breast cancer being one of the most frequently diagnosed malignancies, we turned our focus to chemotherapies commonly used as treatment of breast cancer in an attempt to evaluate the GRC assay as a predictive biomarker across various treatments.
As we had anticipated, the overall incidence of nausea in this breast cancer cohort was higher (31.58%; n = 133) than the reported[9] rate for other solid tumors in a mixed gender cohort. As nausea is considered to afflict female and younger individuals more than male and older, it is not surprising that nausea is more common in this cohort. Patients who demonstrated anxiety over possible CINV symptoms (~10% of all patients) were treated with lorazepam starting a day prior to chemotherapy. In this sub group, patients reported no or mild nausea symptoms only.
Nonetheless, the incidence of nausea based on treatment regimen was as predicted highest in the highly emetogenic anthracycline-based treated cohort (38.1%; n = 42), followed by the TCHP group (36.0%; n = 25). Though there was no significant difference in the type or number of antiemetic agents given prior to treatment, or post chemotherapy, the incidence of delayed nausea was lowest in the TCH group (11%; n = 27) compared to the taxane-based treated group (35.9%; n = 39). The results from the CLEOPATRA trial[36] showed a slight increase in nausea risk for patients treated with the TCHP combination among patients that predominantly were younger than 65 years old without any details regarding mean or median age. Another report of post-menopausal Asian, non-metastatic HER2-postive breast cancer patients, demonstrated no difference between TCH and TCHP in this age group[39]. There are no details regarding prophylactic antiemetics in these two reports comparing TCH to TCHP but the paper by Hussain et al reported an incidence of 8% and 7% in the TCHP and TCH group, respectively, indicating the possible use of similar antiemetic regimens as we report here. In contrast, in our study the median age was 52 years old for the TCHP group [Table 4] compared to 62 years old for the TCH group [Table 3]. The 10+-year age difference between treatment groups might be sufficient to influence the difference in nausea experience.
No significant difference in nausea incidence among Caucasians and African-Americans in either treatment groups was identified. We had no information regarding other reported possible risk factors such as alcohol consumption and motion sickness available in the medical records to test the GRC assay against. Still, since sex and age are considered better predictive factors than alcohol consumption and motion/morning sickness, and the GRC assay, for the most part, outperforms age as risk factor we propose that GRC could be a valuable objective predictive factor for nausea.
The full cohort used in this preliminary evaluation of the GRC assay for predictions of nausea risk among breast cancer patients consist of approximately 200 patients. The first conclusion regarding the GRC assay from this study is that the therapeutic agent outperforms the GRC assay, which contrasts with our previously reported study where the GRC assay was the strongest predictive variable[16]. With this discovery we subdivided the cohort based on the four common regimens for breast cancer treatment. Even though each resulting sub-cohort is still rather small we are encouraged by the results, as they closely resemble the outcomes we previously published for a platinum treated cohort consisting of 64 patients[16] that now has been confirmed in a cohort of twice the size (data not shown, manuscript in preparation) further increasing our enthusiasm for the data reported here.
The CART algorithm identified different cutoff points for each therapeutic agent, allowing for a tailored optimization for each type of chemotherapy, further underscoring that the therapeutic agent is the stronger predictive factor and also acknowledging that each agent in this study has a different mechanism of action that might vary more than the actions of the individual platinum agents in our previous study.
As seen in Figure 1, using the tailored cutoff for the taxane-based therapies improved the accuracy of nausea predictions. As in our earlier study, patients with a lower GRC value, for taxanes between 1.371 and 2.00 (slower recycling of glutathione) were more likely to suffer from delayed nausea than those with a GRC value over 2.00 [Figure 1]. Even though the sensitivity is still low, the specificity and AUC [Table 3] are promising suggesting that this assay might reach values increasing its prospects as a clinical test once we have reached our enrollment goal for the study. To our surprise, for patients treated with anthracycline-based chemotherapy, that generate high levels of cellular ROS[19,40] like the platinum agents previously reported on, the GRC assay did not provide a significant predictive value [Figure 2]. We speculate that anthracyclines could produce subtypes of ROS that might require other neutralizing antioxidants than glutathione. Both specificity and sensitivity for the GRC assay are low when used to predict nausea among patients treated with anthracycline-based regimen. The misclassification rate is the highest among the four regimens and the AUC is below 0.7 [Table 3], further indicating that the GRC assay will probably not be a useful clinical tool to predict nausea for patients treated with anthracyclines.
In the sub-cohort of breast cancer patients treated with TCH only 11% of patients had documented delayed nausea, which considering the small size of the sub-cohort might make it premature to draw any conclusions. At this point, there is a trend indicating that patients with a high GRC (2.539 or higher) are unlikely to suffer delayed TCH-induced nausea [Figure 2]. Again, this result is in line with our previous report.
At this point we do not know the cause for the higher incidence of nausea documented for the TCHP group. Records in the literature comparing TCH to TCHP have shown smaller differences in nausea incidence between these two regimens. However, the median age in our TCHP cohort is about 10 years younger and with youngest patient being only 23 years old. In this treatment group, the CART algorithm determined that sub-dividing the parental node based on age prior to applying GRC as variable improved the accuracy. As seen in Figure 2B, younger patients with a low GRC (below 1.674) were about twice as likely to suffer from TCHP-induced delayed nausea than those with a higher GRC value. Using this approach to nausea prediction resulted in promising values for specificity (0.8125) and accuracy of GRC (AUC 0.7188) [Table 3] signifying a possible clinical application.
In conclusion, while no lab test currently exists to predict a patient’s inherent risk of delayed nausea, we hypothesized that the risk may be correlated with individual capacity to recycle GSH. This early evaluation of our ongoing, prospective study of breast cancer patients has shown that the GRC assay might be a tool to identify individuals at high risk of chemotherapy-induced nausea. As in the earlier study, low GRC value was associated with a high risk of developing chemotherapy-induced delayed nausea for patients treated with taxane- and TCHP- therapies. Of concern in this early evaluation is the misclassification rate. If a patient is undertreated based on the GRC assay, the suffering and possible additional medical visits might negatively affect the patient, their family and work as well as increase medical expenses[8]. There is also a minor risk that the patient will develop anticipatory nausea that is difficult to treat effectively and can result in unfavorable therapeutic outcomes[41]. On the other hand, overtreating patients will result in exposure to agents with adverse effects ranging from mild (headaches and constipation) to more dire (prolonged QT arrhythmia) without any medical benefit in the form of nausea prevention. Though it might seem tempting to suggest glutathione supplementation with over the counter products, large-scale clinical trials of antioxidant supplementation failed to show a benefit[42,43] and rather was associated with a significant increase in cancer incidence and animals studies have demonstrated how antioxidants increase metastasis[44].
Though, not as universally applicable as we would have hoped it appears likely that this assay could support clinicians and healthcare personnel in decision-making processes regarding antiemetics when attempting to tailor prophylactic options for breast cancer patients treated with taxane- or TCHP- regimens to provide enhanced personalized care. Therefore, we have initiated a new, multi center study aiming to validate the assay by obtaining data from a larger cohort with patient reported out-comes information.
Declarations
Acknowledgments
The authors wish to thank all our patients and their families, the medical oncology nursing staff and cancer center phlebotomists for assisting with blood draws.
Authors’ contributions
Conception and design, administrative support: Wallon UM
Provision of study materials or patients: Kennedy J, Ali ZA, Shevade AL, Gilman PB
Collection and assembly of data: McCourt DD, Parikh K, Brady AL, Wang Y, Kennedy J
Data analyses and interpretation: McCourt DD, Buckley ME, Wallon UM
Manuscript writing: McCourt DD, Wallon UM
Final approval of manuscript: McCourt DD, Parikh K, Brady AL, Wang Y, Kennedy J, Buckley ME, Ali ZA, Shevade AL, Gilman PB, Wallon UM
Availability of data and materials
All data were strictly obtained from medical records according to the privacy policy and ethics code of our medical canter.
Financial support and sponsorship
This study was fund by grants from the W.W. Smith Trust and Pennsylvania Department of Health.
Conflict of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Ethics approval for the study was obtained prior to the commencement of the study. Written consent was obtained from all patients involved in this study.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2019.
REFERENCES
1. Warr D. Prognostic factors for chemotherapy induced nausea and vomiting. Eur J Pharmacol 2014;722:192-6.
2. Osoba D, Zee B, Pater J, Warr D, Latreille J, et al. Determinants of postchemotherapy nausea and vomiting in patients with cancer. Quality of Life and Symptom Control Committees of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 1997;15:116-23.
3. Roscoe JA, Morrow GR, Colagiuri B, Heckler CE, Pudlo BD, et al. Insight in the prediction of chemotherapy-induced nausea. Support Care Cancer 2010;18:869-76.
5. Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 2016;66:271-89.
6. Gralla RJ, Osoba D, Kris MG, Kirkbride P, Hesketh PJ, et al. Recommendations for the use of antiemetics: evidence-based, clinical practice guidelines. American Society of Clinical Oncology. J Clin Oncol 1999;17:2971-94.
7. Grunberg SM, Deuson RR, Mavros P, Geling O, Hansen M, et al. Incidence of chemotherapy-induced nausea and emesis after modern antiemetics. Cancer 2004;100:2261-8.
8. Wickham R. Evolving treatment paradigms for chemotherapy-induced nausea and vomiting. Cancer Control 2012;19:3-9.
9. Childs DS, Looker S, Le-Rademacher J, Ridgeway JL, Breitkopf CR, et al. What occurs in the other 20% of cancer patients with chemotherapy-induced nausea and vomiting (CINV)? A single-institution qualitative study. Support Care Cancer 2019;27:249-55.
10. Flake ZA, Linn BS, Hornecker JR. Practical selection of antiemetics in the ambulatory setting. Am Fam Physician 2015;91:293-6.
11. Hesketh P, Navari R, Grote T, Gralla R, Hainsworth J, et al. Double-blind, randomized comparison of the antiemetic efficacy of intravenous dolasetron mesylate and intravenous ondansetron in the prevention of acute cisplatin-induced emesis in patients with cancer. Dolasetron Comparative Chemotherapy-induced Emesis Prevention Group. J Clin Oncol 1996;14:2242-9.
12. Flake ZA, Scalley RD, Bailey AG. Practical selection of antiemetics. Am Fam Physician 2004;69:1169-74.
13. Sekine I, Segawa Y, Kubota K, Saeki T. Risk factors of chemotherapy-induced nausea and vomiting: index for personalized antiemetic prophylaxis. Cancer Sci 2013;104:711-7.
14. Morrow GR, Roscoe JA, Kirshner JJ, Hynes HE, Rosenbluth RJ. Anticipatory nausea and vomiting in the era of 5-HT3 antiemetics. Support Care Cancer 1998;6:244-7.
15. Ihbe-Heffinger A, Ehlken B, Bernard R, Berger K, Peschel C, et al. The impact of delayed chemotherapy-induced nausea and vomiting on patients, health resource utilization and costs in German cancer centers. Ann Oncol 2004;15:526-36.
16. Kutner T, Kunkel E, Wang Y, George K, Zeger EL, et al. Preliminary evaluation of a predictive blood assay to identify patients at high risk of chemotherapy-induced nausea. Support Care Cancer 2017;25:581-7.
18. Janelsins MC, Tejani MA, Kamen C, Peoples AR, Mustian KM, et al. Current pharmacotherapy for chemotherapy-induced nausea and vomiting in cancer patients. Expert Opin Pharmacother 2013;14:757-66.
19. Conklin KA. Chemotherapy-associated oxidative stress: impact on chemotherapeutic effectiveness. Integr Cancer Ther 2004;3:294-300.
20. Yang H, Villani RM, Wang H, Simpson MJ, Roberts MS, et al. The role of cellular reactive oxygen species in cancer chemotherapy. J Exp Clin Cancer Res 2018;37:266.
21. Endo T, Minami M, Hirafuji M, Ogawa T, Akita K, et al. Neurochemistry and neuropharmacology of emesis - the role of serotonin. Toxicology 2000;153:189-201.
22. Leslie RA, Shah Y, Thejomayen M, Murphy KM, Robertson HA. The neuropharmacology of emesis: the role of receptors in neuromodulation of nausea and vomiting. Can J Physiol Pharmacol 1990;68:279-88.
23. Matsumoto S, Kawasaki Y, Mikami M, Nakamoto M, Tokuyasu H, et al. Relationship between cancer chemotherapeutic drug-induced delayed emesis and plasma levels of substance P in two patients with small cell lung cancer. Gan To Kagaku Ryoho 1999;26:535-8.
24. Sanger GJ, Andrews PL. Treatment of nausea and vomiting: gaps in our knowledge. Auton Neurosci 2006;129:3-16.
25. Masella R, Di Benedetto R, Vari R, Filesi C, Giovannini C. Novel mechanisms of natural antioxidant compounds in biological systems: involvement of glutathione and glutathione-related enzymes. J Nutr Biochem 2005;16:577-86.
26. Ishii T, Matsuse T, Teramoto S, Matsui H, Miyao M, et al. Glutathione S-transferase P1 (GSTP1) polymorphism in patients with chronic obstructive pulmonary disease. Thorax 1999;54:693-6.
27. Welfare M, Monesola Adeokun A, Bassendine MF, Daly AK. Polymorphisms in GSTP1, GSTM1, and GSTT1 and susceptibility to colorectal cancer. Cancer Epidemiol Biomarkers Prev 1999;8:289-92.
28. Li J, Zhang D, Jefferson PA, Ward KM, Ayene IS. A bioactive probe for glutathione-dependent antioxidant capacity in breast cancer patients: implications in measuring biological effects of arsenic compounds. J Pharmacol Toxicol Methods 2014;69:39-48.
29. Hendren G, Aponte-Feliciano A, Kovac A. Safety and efficacy of commonly used antiemetics. Expert Opin Drug Metab Toxicol 2015;11:1753-67.
30. Hesketh PJ, Kris MG, Basch E, Bohlke K, Barbour SY, et al. Antiemetics: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 2017;35:3240-61.
31. Bender CM, McDaniel RW, Murphy-Ende K, Pickett M, Rittenberg CN, et al. Chemotherapy-induced nausea and vomiting. Clin J Oncol Nurs 2002;6:94-102.
32. Common Terminology Criteria for Adverse Effects (CTCAE). 2017. Available from: https://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf. [Last accessed on 12 Jun 2019].
33. Song YY, Lu Y. Decision tree methods: applications for classification and prediction. Shanghai Arch Psychiatry 2015;27:130-5.
34. West Philadelphia Census Statistics. 2010. Available from: https://westphillyhistory.archives.upenn.edu/statistics/census/2010. [Last accessed on 12 Jun 2019].
35. U.S. Census Bureau Quick Facts: United States. Population estimates July 1, 2018. Available from: https://docs.vcrma.org/images/pdf/planning/demographics/VC_Quick_Facts.pdf. [Last accessed on 12 Jun 2019].
36. Swain SM, Baselga J, Kim SB, Ro J, Semiglazov V, et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med 2015;372:724-34.
37. Dranitsaris G, Bouganim N, Milano C, Vandermeer L, Dent S, et al. Prospective validation of a prediction tool for identifying patients at high risk for chemotherapy-induced nausea and vomiting. J Support Oncol 2013;11:14-21.
38. Molassiotis A, Stamataki Z, Kontopantelis E. Development and preliminary validation of a risk prediction model for chemotherapy-related nausea and vomiting. Support Care Cancer 2013;21:2759-67.
39. Hussain N, Said ASA, Khan Z. Safety assessment of neoadjuvant pertuzumab combined with trastuzumab in nonmetastatic HER2-positive breast cancer in postmenopausal elderly women of South Asia. Int J Breast Cancer 2018;2018:6106041.
40. Mizutani H, Tada-Oikawa S, Hiraku Y, Kojima M, Kawanishi S. Mechanism of apoptosis induced by doxorubicin through the generation of hydrogen peroxide. Life Sci 2005;76:1439-53.
42. Chandel NS, Tuveson DA. The promise and perils of antioxidants for cancer patients. N Engl J Med 2014;371:177-8.
43. Klein EA, Thompson IM Jr, Tangen CM, Crowley JJ, Lucia MS, et al. Vitamin E and the risk of prostate cancer: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA 2011;306:1549-56.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
McCourt DD, Parikh K, Brady AL, Wang Y, Kennedy J, Buckley ME, Ali ZA, Shevade AL, Gilman PB, Wallon UM. The quest for reliable prediction of chemotherapy-induced delayed nausea among breast cancer patients. J Unexplored Med Data 2019;4:6. http://dx.doi.org/10.20517/2572-8180.2019.01
AMA Style
McCourt DD, Parikh K, Brady AL, Wang Y, Kennedy J, Buckley ME, Ali ZA, Shevade AL, Gilman PB, Wallon UM. The quest for reliable prediction of chemotherapy-induced delayed nausea among breast cancer patients. Journal of Unexplored Medical Data. 2019; 4: 6. http://dx.doi.org/10.20517/2572-8180.2019.01
Chicago/Turabian Style
McCourt, Dillon D., Kinjal Parikh, Amy L. Brady, Yue Wang, John Kennedy, Meghan E. Buckley, Zonera A. Ali, Aarti L. Shevade, Paul B. Gilman, U. Margaretha Wallon. 2019. "The quest for reliable prediction of chemotherapy-induced delayed nausea among breast cancer patients" Journal of Unexplored Medical Data. 4: 6. http://dx.doi.org/10.20517/2572-8180.2019.01
ACS Style
McCourt, DD.; Parikh K.; Brady AL.; Wang Y.; Kennedy J.; Buckley ME.; Ali ZA.; Shevade AL.; Gilman PB.; Wallon UM. The quest for reliable prediction of chemotherapy-induced delayed nausea among breast cancer patients. J. Unexplored. Med. Data. 2019, 4, 6. http://dx.doi.org/10.20517/2572-8180.2019.01
About This Article
Copyright
Data & Comments
Data

 Cite This Article 8 clicks
Cite This Article 8 clicks










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.