A rare case of delayed chronic pneumonitis following non-medical grade silicone injections in a transgender woman
Abstract
We describe a 47-year-old transgender woman with a history of non-medical grade silicone injections given by unauthorized persons 15-20 years prior to presentation who developed interstitial pneumonitis. She suffered acute exacerbations of pneumonitis, developed pulmonary fibrosis with terminal lung disease, acute respiratory distress syndrome and ventilator dependence and died of her illness. In light of the increasing awareness of the health concerns of the transgender population, we review here in the acute and chronic effects of silicone on the lung.
Keywords
Introduction
Silicone has been used for cosmetic augmentation procedures. Local and systemic complications include silicone lymphadenopathy, granulomas, fatal pulmonary hemorrhage, pulmonary emboli, acute and chronic pneumonitis. Acute complications such as pulmonary emboli, pulmonary hemorrhage, and pneumonitis have been reported more commonly than chronic pneumonitis. In cases reporting chronic pneumonitis, patients were either transgender women with human immunodeficiency virus (HIV) or non-HIV patients with autoimmune disease. Here we describe a transgender woman becoming symptomatic 15-20 years after large volume non-medical grade silicone injections in absence of HIV or autoimmune disease.
Case report
A 47-year-old transgender woman was treated for pneumonia 9 months ago when she presented with cough. She had a history of morbid obesity, hypertension, asthma, hyperlipidemia, history of large volume non-medical grade silicone injections 15-20 years ago, ongoing cigarette smoking, previous history of unprotected sexual relations and substance abuse including injecting cocaine, heroin. HIV status, hepatitis B and C titers and Quantiferon testing were repeatedly negative in the past.
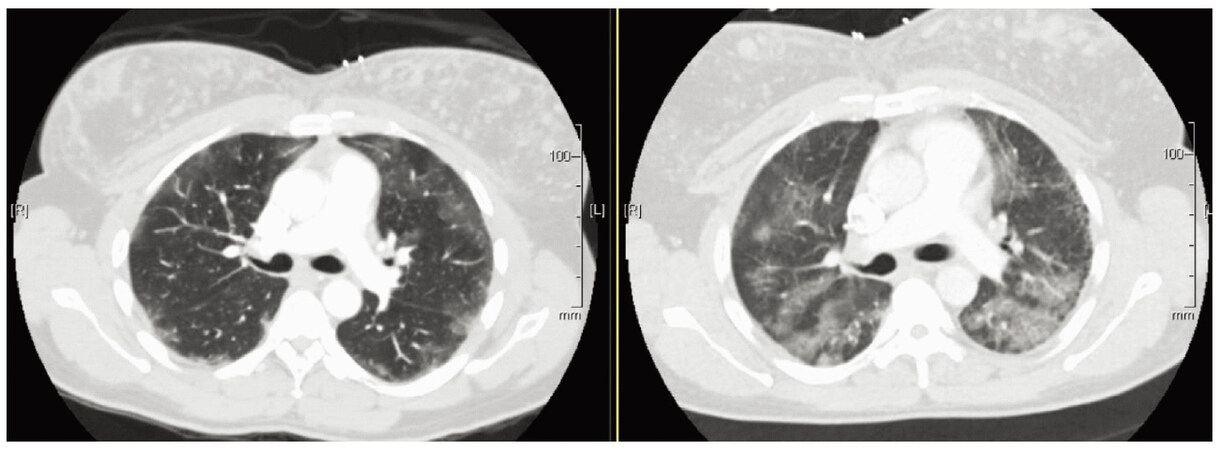
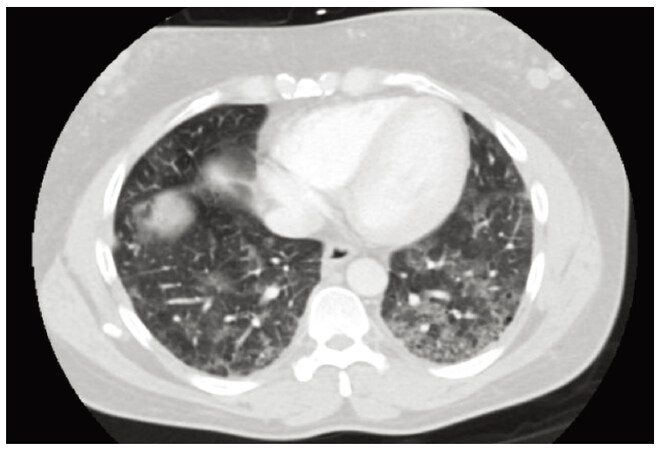
Her symptoms did not respond to oral antibiotic therapy and worsened with dyspnea at rest and orthopnea. She was tachycardic with moderate hypoxemia. Examination revealed a crowded upper airway, bilateral fine rales antero-posteriorly in upper and lower zones. Laboratory investigations showed mild neutrophil leukocytosis. The chest X-ray showed chronic bilateral interstitial infiltrates in mid and lower lung zones similar to chest radiograph from 2007. The patient recalled having mild cough in 2007, and chest computed tomography (CT) showed multiple nodular densities in bilateral breasts, consistent with history of prior silicone injections, with multifocal peripheral upper and lower lobe symmetric ground-glass opacities with patchy interstitial thickening. A chest CT with contrast now demonstrated progression of diffuse bilateral patchy ground-glass infiltrates predominating in the upper and lower lobes [Figures 1 and 2].
Figure 1. Computed tomography chest results (left side, 2007) with worsening ground glass infiltrates (right side 2014)
Etiologies considered were smoking related desquamative interstitial pneumonia, respiratory bronchiolitis associated interstitial lung disease, sarcoidosis, silicone induced pneumonitis, autoimmune pneumonitis, and opportunistic pneumonia. She was treated with antibiotics, intravenous steroids and extensive evaluation with unremarkable autoimmune serologies, HIV screening, hepatitis B and C titers. Bronchoscopy with bronchoalveolar lavage showed 62% macrophages with 20% segmented neutrophils and 10% lymphocytes. Biopsy suggested alveolitis. She was discharged on prednisone taper, oral antibiotics, supplemental oxygen. She was noncompliant with oxygen, smoking cessation. Following steroid taper she was readmitted for recurrent shortness of breath and underwent wedge resection of left upper lobe and lower lobe via video assisted thoracoscopic surgery. Cultures showed no growth, and biopsies showed advanced pulmonary fibrosis with extensive small airways remodeling- airway centric disease, extensive interstitial foreign globular material with numerous lipoid vacuoles consistent with silicone deposition with very minimal normal lung. There were no granulomas or evidence of vasculitis or neoplasm.
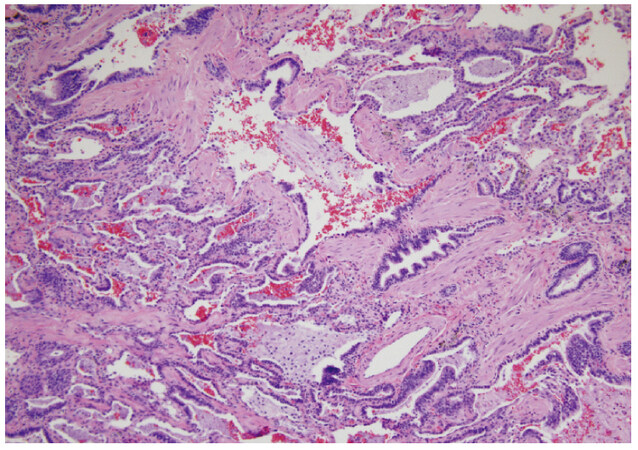
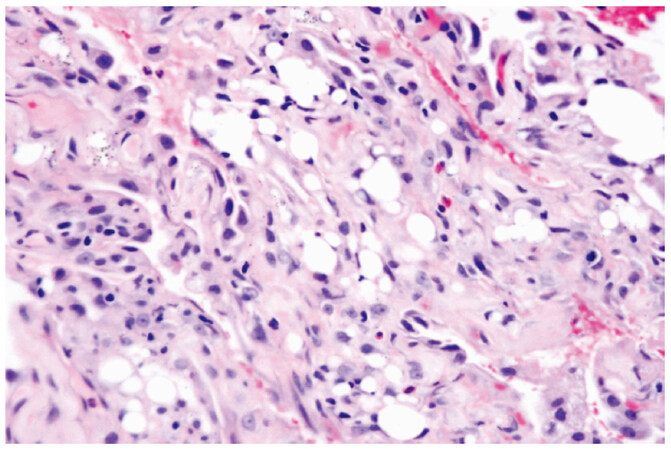
Histology from bronchoscopic biopsy samples suggested alveolitis, peribronchiolar metaplasia, alveolar interstitium with numerous lipoid vacuoles compatible with silicone deposition [Figures 3 and 4].
Figure 3. Alveolar spaces are replaced by metaplastic bronchiolar epithelium (peribronchiolar metaplasia). Magnification 100×
Figure 4. Alveolar interstitium with numerous lipoid vacuoles, compatible with silicone deposition. Magnification 400×
She was managed appropriately after surgery and was discharged with slow taper of oral steroids. However she was readmitted with worsening dyspnea from pneumothorax requiring chest tube decompression, and later was intubated for worsening hypoxia from acute respiratory distress syndrome. Bronchoalveolar lavage collected after intubation revealed acute inflammation with 40% macrophages with 43% segmental neutrophils and 17% lymphocytes. She had a long tenuous course in intensive care unit, on intravenous steroids and broad spectrum antibiotics with worsening hypoxia and given poor chances for recovery, family opted for palliative ventilator withdrawal and she expired shortly after that.
Discussion
Liquid silicone presumed to be inert is used for cosmetic purposes however there are reports of local complications of infection, necrosis and systemic complications of connective-tissue disease, lymphadenopathy[1], and pulmonary manifestations.
The pathologic changes noted in lungs are: (1) intravascular emboli with minimal inflammation[2]; (2) acute pneumonitis with edema/hemorrhage leading to acute respiratory distress syndrome[3]; and (3) chronic pneumonitis.
Number of silicone injections, amount of silicone and contaminants associated with silicone determine degree of inflammatory and fibrotic response. Clinical course is determined by pathological changes in lungs and host immune responses. There are multiple case reports of acute pneumonitis, silicone embolism, alveolar hemorrhage however there are only few case reports of chronic pneumonitis. Majority of chronic cases are seen in transgender woman with HIV infection as was reported in 2 case reports[4,5] or related to development of autoimmunity[6] as was reported in a woman 30 years following mammoplasty[7]. There is 1 case report of a patient developing pulmonary fibrosis 5 years after silicone injections with relatively stable disease[8]. To our knowledge, this is the first report of a patient presenting with symptomatic lung disease 15-20 years following multiple non-medical grade silicone injections with no evidence of HIV or autoimmune disorders. Her severe presentations were most likely due to silicone induced pneumonitis/chronic fibrosis with some contribution from smoking. Pathology also supports changes due to silicone such as interstitial globular material deposition with vacuoles, peribronchiolar metaplasia. After becoming symptomatic, she remained steroid dependent with continued worsening leading to terminal lung disease, ventilator dependence with very high oxygen requirements and death. Continued education of transgender community about side effects of non-medical grade silicone is henceforth required.
Declarations
Authors’ contributionsConception and design of the article: Sridhara S, Sivaswami S
Manuscript drafting and editing: Sridhara S, Baksh M, Reddy V, Norwood S, Sivaswami S
Literature research: Sridhara S
Final version approval: Sridhara S, Baksh M, Batool K
Financial support and sponsorshipNone.
Conflicts of interestThere are no conflicts of interest.
Patient consentThe patient’s sister who is the medical power of attorney provided their informed consent for publication.
Ethics approvalThe work has received the approval by our Ethics Committee.
Copyright© The Author(s) 2018.
REFERENCES
1. Alva RV, Yacoub WJ. A young woman with pulmonary hemorrhage and hypoxic respiratory failure. Chest 2010;137:484-7.
2. Schmid A, Tzur A, Leshko L, Krieger BP. Silicone embolism syndrome: a case report, review of the literature, and comparison with fat embolism syndrome. Chest 2005;127:2276-81.
3. Pastor E, Andreu AL, Chiner E. Acute pneumonitis and adult respiratory distress syndrome after subcutaneous injection of liquid silicone. Arch Bronconeumol 2005;41:702-3. (in Spanish).
4. Hariri LP, Gaissert HA, Brown R, Ciaranello A, Greene RE, Selig MK, Kradin RL. Progressive granulomatous pneumonitis in response to cosmetic subcutaneous silicone injections in a patient with HIV-1 infection: case report and review of the literature. Arch Pathol Lab Med 2012;136:204-7.
5. Chastre J, Brun P, Soler P, Basset F, Trouillet JL, Fagon JY, Gibert C, Hance AJ. Acute and latent pneumonitis after subcutaneous injections of silicone in transsexual men. Am Rev Respir Dis 1987;135:236-40.
6. Pineda JC, Díaz JC, Agualimpia A, García JF. Autoimmune/inflammatory syndrome induced by adjuvants causing myositis and pulmonary fibrosis. Isr Med Assoc J 2013;15:720-1.
7. Miyata Y, Okano R, Kuratomi Y. Interstitial pneumonia associated with human adjuvant disease which developed 30 years after silicone augmentation mammoplasty. Nihon Kyobu Shikkan Gakkai Zasshi 1997;35:1093-8. (in Japanese)
8. Huynh TN, Yochim SE, Martin SP. Case in point: silicone-induced pneumonitis in a transgendered patient. Available from: http://www.psychiatrictimes.com/authors/nader-kamangar-md#sthash.EBT5f8Ha.dpuf. [Last accessed on 8 Dec 2017].
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Sridhara S, Baksh M, Batool K, Chowdhury J, Reddy V, Norwood S, Sivaswami S. A rare case of delayed chronic pneumonitis following non-medical grade silicone injections in a transgender woman. J Unexplored Med Data 2018;3:1. http://dx.doi.org/10.20517/2572-8180.2017.20
AMA Style
Sridhara S, Baksh M, Batool K, Chowdhury J, Reddy V, Norwood S, Sivaswami S. A rare case of delayed chronic pneumonitis following non-medical grade silicone injections in a transgender woman. Journal of Unexplored Medical Data. 2018; 3: 1. http://dx.doi.org/10.20517/2572-8180.2017.20
Chicago/Turabian Style
Sridhara, Srilekha, Mizba Baksh, Khatja Batool, Juel Chowdhury, Vijay Reddy, Stephanie Norwood, Sivaraman Sivaswami. 2018. "A rare case of delayed chronic pneumonitis following non-medical grade silicone injections in a transgender woman" Journal of Unexplored Medical Data. 3: 1. http://dx.doi.org/10.20517/2572-8180.2017.20
ACS Style
Sridhara, S.; Baksh M.; Batool K.; Chowdhury J.; Reddy V.; Norwood S.; Sivaswami S. A rare case of delayed chronic pneumonitis following non-medical grade silicone injections in a transgender woman. J. Unexplored. Med. Data. 2018, 3, 1. http://dx.doi.org/10.20517/2572-8180.2017.20
About This Article
Copyright
Data & Comments
Data
 Cite This Article 1 clicks
Cite This Article 1 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.